Last night, I was noodling around on-line and discovered, much to my delight, that Jim Gilliam, one of the co-producers of Outfoxed: Rupert Murdoch's War on Journalism, had noticed my little "review" of his documentary. Unfortunately, my delight turned to despair when I saw that I had left off the last "e" in coffee, I could have used a comma between "pooch" and "put", and the sentence that starts "They had put a blackboard out that they planned to hold.." is just grammatically sloppy. I guess asking Mr. Gilliam if he has any jobs available in production would be overly ambitious, at best. (Sigh...)
In other news...
The CommercialCloset.org, a popular Web site that chronicles the use of gay and lesbian images in advertising, was shut down on Wednesday after it was believed to have been the victim of a cyber attack by the American Family Association, one of the nation’s largest anti-gay lobbying groups, over the use of a pro-gay ad produced by Procter and Gamble. Read on...
I love the part at the end of the article about how the hate mail was illiterate. The only uplifting part about a similar on-line attack against Margaret Cho was the people writing in seemed borderline retarded. I am a (newly) proud investor in P&G. Despite my current precarious financial state, I won't be selling.
Manhattan judge strikes down section of Patriot Act. "Here, you can have a tiny fraction of your inalienable rights back."
Are you Happy in Vancouver? It may only be local to "the gays" in British Columbia, but that's the secret code they use to find out your status. Get it? Happy in Vancouver. - via buggery.org
I am totally 429. This one's a stretch. You have to check your phone key pad. 4 = ghi, 2 = abc, 9 =wxyz. Europeans, go figure. - via Steph & Alek
Here's some more 411. Some may say T.M.I. but what the hell ....
In my continuing effort to bring relevant HIV information to people (like me) who need it, I frequently stumble across things that I never knew, I never heard discussed. And I'm always amazed and a little pissed off. I guess I should just be glad the information is out there for me to find. For example:
I had no idea that Sustiva and indeed many other commonly prescribed HIV meds can cause moderate to severe depression, anxiety and in some cases psychosis. People already dealing with problems like this should be made aware of the possibility before beginning treatment so at the very least, if you feel a severe depression or other psychological changes start to happen you would know where to begin looking. I only became aware of it from seeing doctor/patient questions posted on-line.
From another forum where someone just beginning treatment and complaining of dehydration asked for advice, I found out that just being HIV+ (without meds) can cause dehydration or cause you to feel extreme thirst. So the extreme thirst and dehydration I've been feeling for over three years is probably not all in my head but real. Seriously. I have water with me all day. Every day. I drink on average 4-6 pints of water a day. I thought it would go away once I quit smoking. It didn't. I thought it was from drinking and while that made it worse, my current end of the night Stoli/soda (or two) wouldn't be enough to cause it. Dehydration is a common issue with the HIV virus. Just in case anybody else is walking around totally parched all the time and thinking you're a tad crazy.
And lastly, at the risk of embarrassing myself completely once and for all:
"Hello, my name is Tom and I fart."
"Hi, Tom."
My story goes something like this. Up until (again) about three or four years ago, I was a normal farter. The occasional fart at night on the couch while watching a video. My farting was what you would expect of a normal human who farts normally. Usually pretty harmless, once in a while quite odiferous. If anything, the only remarkable thing about gasses escaping my body against my will is that I hardly ever burp. I don't supress them I just don't burp. But all that has changed. The last few years I have been uncontrollably flatulent. Well, not uncontrollably, I guess. I can in fact control it if I have to. Usually in the morning and then again at night (anywhere from 10pm on), I become the gassiest gassbag from Gassville, USA. I fart. Loudly and repeatedly. Sometimes for hours.They are frequently big, tremendous, rumbling farts from deep in the land of Big Fartville. Usually about fifteen minutes apart in time. Sometimes I doubt that a human can carry around as much gas as I expel.. And it does seem to be just gas. There's no pain, and usually no "unpleasantness", just air. Lots and lots of air escaping my butthole with a thunder reserved for Thor himself. I would frequently have to go into my office at work (when I had a job) and just rip a few off for an hour or so. I would try to time a paperwork task, like payroll, to my volcanic sphincter so I could calculate and fart at the same time. I'm a good multitasker. I thought it was a getting old thing. Funny though, as much as my uncles and Dad freely discussed prostate and various urinary problems, I'd never once heard them mention exploding the buttseam on a pair of pajamas as a side effect to aging. Turns out, the real culprit may be my old pal HIV. This article has all the information including this salient point:
First, HIV itself can contribute to intestinal gas. HIV naturally gravitates towards the gut, which provides a hospitable environment for the virus. A high viral load in the gut will disrupt normal functions and can result in gastrointestinal distress -- a polite way of referring to diarrhea, nausea, vomiting, and gas.
So the next time you're in the gym and the guy next to you is doing crunches, and just as he's quietly calling out number 29 he loudly rips a huge fart, don't laugh. He may be HIV+. Thankfully, I haven't been seeing anyone these last couple of years. (There's a sentence that was painful to write.) Leaving me free to fart at will in private. A closet farter, if you will. But now you know my secret shame.
My brother and his wife arrived Thursday afternoon for what has turned into an annual visit to New York City. This would be the third year in a row. I have finally learned that it's impossible for me to arrange for them to be entertained each and every day, so I have gradually stopped trying. Not enough really seems to interest them, or rather, interests both them and me for us to do together, so now, rather then give myself whiplash trying to bend over backwards to please them, I simply make a couple of plans and see if there is any interest. If they don't want to, they don't want to. And if I don't feel like joining them, I don't.
So it was that Thursday afternoon after checking into their hotel room they immediately left for Yankee Stadium and an afternoon game. I decided not to attend. I've been to Yankee games in the past and enjoyed them but I'm holding out for a new experience like a seat in a luxury box or right behind home plate. "Baseball player butt" mmmmmm. I met up with them around 9 pm after I had a pre-interview job interview. We'll see what comes of that. Typically, my brother and his wife didn't seem to want to do much of anything. So we sat in a building common area on 51st/Broadway and chatted about the family, jobs, their new grandchild etc. Eventually we walked down to 42nd St. and looped around to 8th Ave near their hotel. I noted they've opened a Swatch outlet on 45th/Broadway and filed that under "future shopping". I loves me some Swatch watch. We talked for a while on the street, made plans to meet up at some point the next day and that was that.
Friday, they made their way up to Riverside Park for a while until I met up with them that afternoon back at the hotel. I had been wanting to check out the new Time Warner complex since it opened and never got around to it. This seemed like a perfect time, as the one thing all the males in my family do enjoy doing is walking around looking at gigantic retail operations. Casinos, theme restaurants, shopping centers, wherever large construction projects and commerce have blended together, all the men in my family like to have a look. I'm not sure if the women share this trait, or adapt to survive what could be misconstrued as crushingly boring.
I have to say, just from the outside, taking in the enormity of the complex is rather breathtaking. It has had it's detractors since completion but I think it's a beautiful structure.

Inside, it was a shopaholics (me) wet dream. Hugo Boss, Armani Exchange, Cole Hahn, Williams-Sonoma and a just opened Samsung display area with all their latest and greatest cell phones, portable DVD players, laptops, washer/dryer combos (in a single unit) and internet access reproduction's are on display in various "household" settings for you to try and presumably buy. But it was the Whole Foods Market on the basement level, that was the crown jewel in this excursion. It was a chaotic (on a Friday afternoon!) cacophony of young and old, rich, hip and bohemian blend of humanity all with one thing on their minds.... spend money good. And this market is set to accommodate you any way you please. Aside from typical grocery fare they have the largest organic section of anywhere in Manhattan bar none. In addition they have three different salad bars, a select your own pizza station, packaged sushi or made fresh to order, both a hot and separate cold soup station, they had one salad bar station devoted specifically to olives, all kinds of olives. Pre-packaged dinners, sides and side-salads. You can take it to go or they provide a seating area if you want to just come in for lunch. As long as you buy it there you can eat it there. They even provide a microwave if your food needs to be re-heated. Conveniently, Jamba Juice has opened a franchise inside. I've been reading various postings about the magical qualities of the Jamba for months , so of course, I had to try. It was delicious, but seriously kids, it's a smoothy. Sure, you can get things added to it that may or may not do you any good (like extra vitamins or fiber) but is this thing gonna make you smarter or better in bed (as their signage suggests)? Don't think so. It's a smoothie. They can only do so much.
Thoroughly impressed, we were due to meet up with my cousin and his wife and besides, I was having a baby sized panic attack. My throat felt like it was closing up and I kept obsessively swallowing which of course, causes your throat muscles to fatigue which of course, makes it feel like your throat's closing up. Feedback loop. A classic panic symptom. I have a couple of theories as to what caused it which I may or may not get around to discussing later, but I had already decided, rather than suffering needlessly, I would keep the medication for panic close at hand. Dose first, ask questions later. That's my new motto. I took a Clonazepam as we were heading over to Mickey Mantle's on Central Park South to see if they had any souvenir T-Shirts in the gift shop. By the time we were heading for the subway downtown a half hour later, the compulsion and panic had vanished. Chemicals, yay!
We met my cousin and his wife on 14/7th and the location for dinner got tossed over to me. I threw out a few suggestions. When I mentioned a great burger joint I had eaten in recently just below St. Mark's on 2nd, I saw enough eyes light up that I decided to lead on. Simple folk, simple food. I wish I could tell you the name of this place, and I want to say it's Paul's, or Bob's or something very non-descriptive, but really it's just below St. Mark's place and it's absolutely lousy with neon and signage (the word of the day) declaring the greatness of their burgers and I'll be damned if it isn't true, they make a damn good burger (the hair in my cousins food notwithstanding). After dinner we waddled up to my apartment so I could walk the dog. All four of them declined my invitation to walk up five flights to my apartment and I decided mentioning that I usually do it four times a day, if not more often, would be needless bragging on my part. Notice it didn't stop me here. After dinner, I led them to a funky coffee shop (Push Cafe if you want to try out the Blog Search feature) that turned out to be closed for the Jewish holiday. Jews own coffee shops, who knew? So we settled in to the nearby Lyric Diner for coffee and dessert. Our waiter was tall, lanky, foreign and *sniff* about 8 1/2 uncut, I would say.
Saturday night included a trip to The San Gennaro Festival. Crazy on a Saturday I know, but not my idea. It was as expected a cluster fuck. This year we skipped dinner first as last year, while dinner was enjoyable, it made it impossible to try all the food for sale along the way. I mean, I like to eat but... So it was with gluttonous abandon that I enjoyed calamari, fried shrimp, sausage and peppers, a bowl of meatballs, two glasses of fresh squeezed lemonade and a pineapple/strawberry smoothie. We walked the entire length of the festival, and then the entire length in the opposite direction. Looking for sweatshirts. Specifically dark green sweatshirts that had The Feast of San Gennaro, Little Italy, NYC embroidered on them. Apparently, someone from last year's excursion returned with just such a sweatshirt. My Mom and Dad liked it so much, they pre-ordered it as a souvenir from this year. My brother has a hero complex to rival my own, so this was not a mission he was prepared to fail at. Had we found the sweatshirts at any time on the way back, we would have been out of there. As luck would have it, the only booth selling the correct color sweatshirts with the correct embroidered information were on the very first block of the festival. Triumphantly happy, we could leave for a less crowded location (read: anywhere else). I led them out of Little Italy and up to the East Village and into the New York Milkshake company
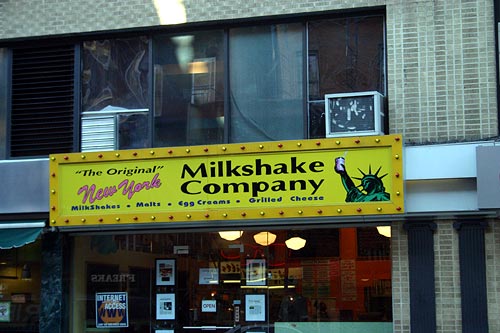
where you can order a milkshake (naturally) and also grilled cheese sandwiches and fried peanut butter and jelly (which I haven't tried yet but I must). I topped my salute to gluttony with a root beer float. We ended up walking up to Union Square and pulled up a bench in the park. My brother ended up chatting with my cousin and his wife while I regaled my sister in law with tales of how I came to know and live with The Hellcat. At some point early on, a pregnant 22 year old heroin addict took the bench next to ours. After bumming a cigarette and a light she promptly fell asleep and dropped the lit cig onto her coat. Causing my cousin's wife no end of distress. I turned to my brother and said "It'll probably go out.... or she'll start on fire. Either one." Finally, some college kid frolicking over the benches landed hard enough to roust her, at which point my cousin alerted her to her imminent danger. The my cousin's wife suggested that the pregnant 22 year old heroin addict should put out the cigarette she had just bummed. If looks could kill my cousin's wife would be incinerated.
Long Post. I've asked quite enough of you for today. Tomorrow: My long awaited trip to Coney Island (and more pictures)
One a you scabby bastards could have told a person my blog was displaying funny in Internet Explorer. It looked fine in Mozilla.
A new week begins in the morning. The Hellcat is returning from his West Coast Tour. Should be interesting to see how badly I get thrown over by Colby now that "real Daddy" is back. Men.
The Ex is returning from Folsom Street S.F. I'm sure I'll be regaled with endless stories about people naked in public and how his friends all didn't get along.
The job search kicks up a notch as entertaining the famiglia all weekend tore a hole (hehehe hole) in my pile o' cash.
I'm gonna try and write some good stuff this week. I promise. I feel like I've been coasting.
Just having the chemicals in your pocket that you know will solve the problem... solves the problem. Amen.
I was three quarters of the way though the story of my bother and his wife visiting for the weekend. It was kind of funny and sarcastic and full of links. Then the Mozilla browzer stopped responding and in trying to close a page I closed everything and lost the entire post.
My brother and his wife are visiting Manhattan for the weekend. We're having an OK time. My cousin and his wife have been joining us. They live down on Wall St. Maybe I'll try to re-create the post if I have time tomorrow. But I doubt it.
Did a photo shoot yesterday. He described himself as 5'8 160 with a muscular athletic build, he described his chest as hairy, but trimmed. The picture he sent was with his chest untrimmed and if you remember the few pictures I've posted of other photography subjects, he was far and away different than anyone I had photographed before. He also wanted to shoot in black and white. I like black and white photos. But usually I shoot in color and then Photoshop the color out if I want to see the image in greyscale. So I was excited because there were several challenges.
I found out late in the shoot that he's straight. Or at least bi, as he spoke of his girlfriend. If he was straight he was about the most comfortable straight man around a gay photographer I could imagine. After we talked for a bit and talked about ideas for shots and I explained my process as far as coming up with ideas for shots we began the session. Tank top and board shorts on the couch. He lifted up the tank to show his abs, then later his chest. Without me asking. Very hot shots. I asked him to put one arm and then both back behind the couch arm. I have an armpit fetish and I know for a fact I'm not alone.
I asked him to change into something else and he picked a pair of Calvin Klein boxer briefs. I managed to get one shot of him mid-change that he didn't even notice but afterward we both agreed it was candid and fucksexy.
We talked about photography and what we thought made sexy pictures and general bullshit about how long I've been doing this and how craigslist is full of freaks and wierdos but every once in a while you meet someone who is what he says he is. I did a variation of some reflection shots a la him in my living room mirrors, but they were focusing more on the mirror as opposed to the face. I got a great shot of him taking the tank off up over his head with his arms up and his chest and tummy exposed in duplicate that came out fucking awesome.
We went to my bedroom for the nude shots. Not because I was looking to get a little but because I have a pretty cool bed for photographs and because I get this really interesting light effect in the afternoon through my bamboo shades. I photographed him stripping down in stages. Once he was naked he started jerking, not off, but sort of self fluffing. No dummy this one. He had a hot cock but he was just presenting in the best possible light, as it were. A policy I wholeheartedly support. In any case he was driving me nuts.
We did about fifty shots and managed to work through a camera malfunction where we lost a bunch of shots. I'm going to have to replace my digital soon as it seems to have some software flaws I don't think are solveable. In spite of that, I printed and saved six shots for my portfolio that I thought came out great. That's a record as I usually only think two or three are worth saving.
I asked him towards the end as he absentmindedly tugged on his half hard cock if he was going to "go for it". He said no, he hated those hard cock j/o shots.
"O.K." I said. And started setting up for some final shots.
"You want me to?" he asked.
"Of course. But if you dont want to do it it's fine."
He started playing with his dick and then said "hang on" and left, I'm assuming to lube up as he didn't return with a cock ring or butt plug, after which he managed to get his dirty bits impressively hard, which I recorded for posterity. Turned on and satisfied, I pronounced the session over and showed him the computer shots and burned them to a disk. He thanked me, hugged me, and went on his way.
All in all a nice afternoon and as an added bonus, it seems he's a masseur ( I guess that explains the nudity comfort he showed) and he's offered a free massage for me in return. You know I will take him up on that offer ASAP. I wish I could post all of the six pictures I like but I must protect his image as I have no right to expose him on-line. Still, I got a couple that I can post without breaking a trust. If you ever want to set up a session let me know. I can get you some good hot photos. Or, I can take your picture, get you naked and do dirty stuff with you.


Evangelist (and prostitute fucker) Jimmy (I have a tiny penis) Swaggart apologizes for saying he would kill gays.
I said it first: Sex and The Clitty.
|
| From: "Thomas Tricoli" <tommyrico@msn.com> To: a######777@hotmail.com Subject: RE: let me know Date: Fri, 24 Sep 2004 00:30:30 -0400 ????????? |
To: tommyrico@msn.com
Subject: RE: let me know
Date: Fri, 24 Sep 2004 00:32:01 -0400
i responded to your ad on craigslist.
Can u send me more info about you
| From: "Thomas Tricoli" <tommyrico@msn.com> To: a######777@hotmail.com Subject: RE: let me know Date: Fri, 24 Sep 2004 10:39:20 -0400 No. Because you're too dopey to know that I have more than one craigslist ad so I have no idea what you're responding to. You're very strange.... Why would you think that anyone would respond to an e-mail with "let me know" as a subject and absolutely no information whatsoever? Let you know what? About what? Who are you? What do you want? Sex? Do you imagine that could happen without a scrap of information of any kind as to who you are or what you look like? Anything? Do you live in a vacuum? Are you stupid or just a complete freak? I'm just totally curious why you would even waste the second it took to send me something of no value or interest whatsoever. |
| |
| |
Posted a sex ad this afternoon looking to give a NSA blowjob. Sometimes I'm just really into getting another guy off. I get all my pleasure literally out of giving pleasure. Sometimes. He came over around 4. By 4:10 we were naked on my bed. He was sort of my type. Latin but 30ish. Stocky but by no means fat. He will be fat in ten or fifteen years though, guaranteed. Armband tattoo. If I saw him in the gym I would guess straight. Not straight, though. Sooo not straight. We we're kissing and jerking. He seemed to like jerking me off. He tweaked my nipple. Am I the only fag that isn't into having my nipples played with? It does absolutely nothing for me. Having said that, if we're in bed and you lightly brush your fingertips across my belly and up my chest and brush a nipple, your reward will be an instant eraser nub, gooseflesh everywhere and a soft moan from between my lips. (And I'd probably cook you dinner.) He had a nice cock. Not huge about 6 1/2 with a big fat head. And cut. A cut latin man. They do exist and they really are my favorites. I spit-lubed my hand and started to stroke him. There's my little moan. A few minutes later I decide to get what I brought him over for and engulfed his cock. There's my big moan. I went right to work, alternating hand and mouth strokes, using just my hand when I started to get tired or bored. I didn't speak. A couple times I took my mouth away and looked him in the eye, a wicked grin on my face. He was enjoying this too. After a while, he reached down my back and played around outside my hole. I liked it, but decided not to send the "go ahead" signal. This was about me sucking him off. It's all I wanted. After about 10 minutes or so, his moaning got progressively louder and he leaned back on his arms. He moaned loudly and lightly pushed at my head to let me know he was close. "Thanks man" I thought, "but we're going all the way." He got the message and went for it. I don't need to get the load but really, if you're gonna play the part of total cocksucker why not get the total experience. Pretty soon we had passed the point of no return and he was moaning and sucking air. After four or five strokes I pushed myself all the way down on his cock and just stayed there, letting him finish. Satisfied, I finally pulled off, wiped my mouth with the back of my hand and said, "Thanks, man".
"No" he said, "thank you."
He got dressed and left. I got ready to hit the gym and do some cardio. Oh yeah, then I called my Mom.
I had a meeting at GMHC today to see if I might be eligible for any kind of gummint cheese or da' welfare or some such thing. Not that I'm destitute or anything but I'm trying to be proactive in case the money runs out before I find a new job. Unfortunately, they have informed me that while yes, I am in fact a gay man, and yes, I do have ongoing health issues, (For those of you new to the party, I have a currently incurable viral infection coursing through my bloodstream which, if untreated when the time comes for such action, would probably kill me.) my current financial picture does not officially constitute a "crisis". So I was given several nicely printed informative pieces of paperwork explaining what a true "crisis" really is, some not so helpful but much appreciated job placement information, and if I'm not mistaken an implied pat on the head followed by a swat on the fanny and an unspoken "on your way now, you scamp." The saga continues...
I have a photography session set up for tomorrow afternoon. The subject is early 30's around 5'8 with a hot hairy chest and a lean muscular bod. Unless the picture he sent is total bullshit. But I have a good feeling..... I'll let you know. Hey, it beats looking for work.
I'm trying to adjust my body clock to a real-world workday friendly 9-5 rhythm. It's around 1:30 am. I ain't tired. Perhaps a martini... (Hey, it beats a cheap-ass $3.99 bottle of Andre.)
Britney spits out her gum long enough to say "I do". And with that, she becomes stepmom to two illegitimate children. But there was so much more. It seems the now brunette Britney, insisted her father go to rehab to kick an addiction to booze and painkillers, as she expressed her wish that she wanted him "sober enough" to walk her down the aisle. How does one define sober enough down on the bayou? So, after arranging for the entire wedding party to change into velour tracksuits emblazoned with "Pimp" and "Pimp Daddy" (classy) it was off to the reception where guests dined on chicken fingers, ribs and salad. I'm told they had a choice of dipping sauces and that each meal came with a toy surprise.
Evangelist (and prostitute fucker) Jimmy (I've got a tiny penis) Swaggart Threatens to Kill Gays.
I'm heading out to pick up an order of contac lenses. I've been using Cohen's Fashion Optical (108 E. 23rd @Park Avenue South). In fairness, the service is always fast, efficient, and you get exactly what you're expecting when. Then they steal from you. The last time I went it was for a new pair of glasses. I had some extra money and wanted to make a change so, carrying about 250.00 with me I went in. I exited an hour later having spent close to $400.00. After selecting the frames and then the special shatter proof lenses and then the iodized crystallized jelly inserts (or something) final cost: almost double what I figured on paying. So it's no wonder I've been ordering my contacs on-line. But in between the last time I ordered and now, a law has taken effect that you have to have your optometrist confirm your prescription. So I dutifully filled out my order form including the phone number and address of Cohen's Fashion Optical (108 E. 23rd @Park Avenue South). Hours later I received an e-mail from the company stating Cohen's is claiming my prescription has expired and they couldn't fulfill my order. Annoyed but not surprised, two days later I stop into Cohen's Fashion Optical (108 E. 23rd @Park Avenue South) and say that I want to order new lenses. This would be the part where she would recommend a check-up right? After all, my prescription has expired.
"How many boxes would you like?"
"That depends, how much are they?"
"It's four boxes for $100 but if you take out the $150 insurance it's six boxes and I'll throw in the extra two boxes on this order. So what would have cost me $87 on-line has now set me back $250, and once again I leave this business feeling raped. Oh, and did ya notice? Not word one about my "expired" prescription. But I do get free contac solution. But I have to ask for it. I'm guessing there will be a "storage" charge.

Home Alone star arrested in Oklahoma for drug posession. Do you think Michael Jackson still wants to suck his dick? I sorta do now.

James St. James posts his notes after doing crystal meth.
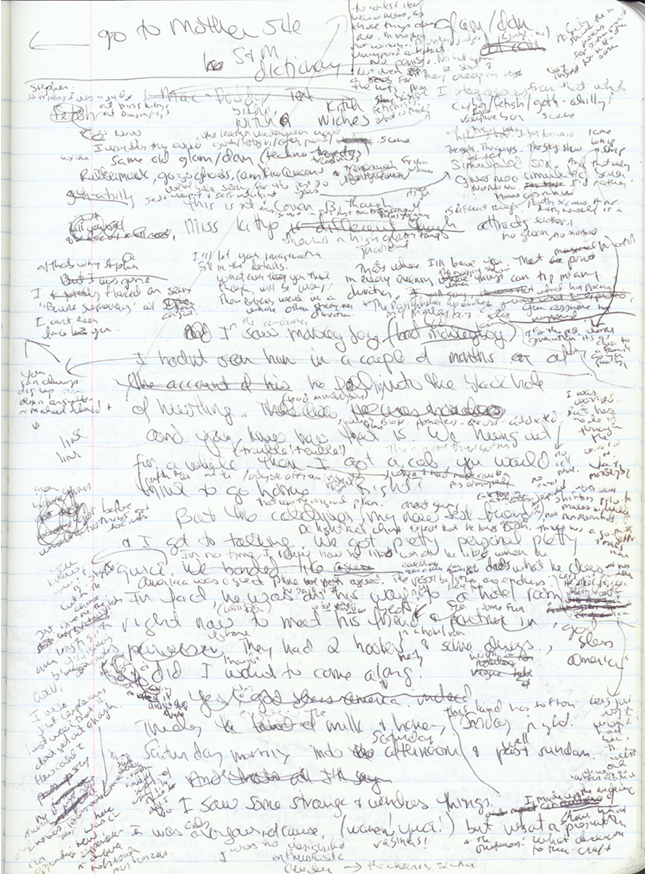
This looks like a fun headspace, huh?
With myself. Getting fired has highlighted a serious problem for me. Short term, I knew what I didn't want to do. Work there anymore. In general, I know what I don't really want to do. Work in a bar/restaurant. It's been seventeen years. Enough. I can't deal with the drinking and the drug problems and the back stabbing. Quite frankly, I'm getting too old. 3 years at God's Waiting Room has left me feeling dead inside. If I didn't have this chronicle as a creative outlet I would have surely descended into madness by now.
I've spent the last week puttering around Manhattan, busying myself tanning, renewing my contac lens prescription (remind me to talk about that), shopping, having my ass waxed. I've been trying to stay in shape by at least getting a half hour of cardio every day. Add in at least four trips up and down, well, down and up five flights of stairs to walk Colby (for this effort he rewards me by pissing or shitting in the apartment at least once every day, no matter how I try to outsmart him) which I'm counting as exercise, food shopping, laundry. I've been cleaning the bathtub with a new cleaner I found, trying to get the porcelain back to a pure white. I still haven't gotten around to the big kitchen clean-up I've been trying to take care of.
The whole time, I've been in conversation with my inner voice. My inner voice talks to me a lot. Mostly it asks me repeatedly "how do you feel?" My inner voice monitors my body and my feelings all day every day. Sort of my privilege as a gay man. Since I have no kids. Since my family is in another city. Since I don't have my own pet (sorry Colby). Since I don't have a boyfriend. It's me. Me, me, me. How do I feel? I'm hot, do I have a fever? My blood sugar feels low. Should I eat now? Why is my back sore? I'm horny. I'm horny a lot. Are my anxiety meds working? Am I anxious? What does anxious feel like, really?
But lately my conversation with my inner voice has been on repeat. And it keeps repeating "What do you want to do?". And so far, my only real true answer has been, I have no idea. I know very clearly and confidently what I don't want. But what the hell do I want? And how do I figure it out? And then how do I get it?
Ex-porn king trades sex for salami

Villager photo by Elisabeth Robert
Jack Lebewhol, left, owner of the 2nd Avenue Deli, with one of his newest employees, Al Goldstein, who used to publish Screw magazine and now works for $10 an hour. "I've always preferred food to sex," Goldstein said.-via The Villager
My love for Miss Martha is well documented. But I caught the entire press conference yesterday afternoon and if I had been drinking at the time, I counted at least four instances that would surely have resulted in a spit-take. The lady has got balls, man.
From a positively gigantic podium/stage flanked by her drones, Queen Martha proclaimed, "I must reclaim my good life. I mut return to my good works." Yeah, OK Ghandi. Lady, you make radish flowers. While you are making the world more tastefully arranged, you're not the cure for cancer.
In an unbelievably transparent mis-use of the elderly Martha trotted out the spirit of her 90 year old mother as a means of convincing the judge to let her serve her time in the Danbury prison nearest her home. She then proceeded to talk of her devotion to her "two beloved, fun-loving dogs, seven lively cats, horses, canaries and chickens." Chickens? They're making you leave behind your chickens? Oh, the humanity! Hey Martha! Don't you have a daughter you might want to work in a mention to? What the hell was her name again? "Hey you"?
Then there was this bit of wierdness: "America accounts for 25 percent of the world's prison population, despite the fact that we have just 5 percent of its population. I will be joining more then 2 million other souls who are serving time." Well, not exactly, Martha. You're headed for five months in minimum security, followed by 5 months in your own multimillion dollar mansion. It ain't OZ.
She even managed to drop in a pitch to advertisers urging them to return to her magazine. I guess that's why I heart Martha. She's got absolutely no shame.
Rick James' cause of death due to an enlarged heart, pneumonia as well as Valium, Xanax and Vicoden
Oh, and Robbie Williams claims he's not gay and he might sue. Don't bet on it.
Eminem Nude!
I have to admit, he's got a nice butt.
I think I'm blogstipated. I can feel them in there. I've got a lot to write about. There's the story from my trip to Buffalo, "The Reveal". The story of my total and utter confusion regarding finding a new job. The story about being jobless, and still incredibly busy at the same time. There really aren't enough hours in the day after all, go figure. But I go to the "create post" page and I just ... can't ... seem to ... squeeze one out. But by all rights I should be writing my ass off shouldn't I? I have a lot to say and extra time to say it, so what gives?
Instead all I can manage are tidbits:
- I enjoyed my first Sunday off in a loooooong time. I went to brunch. Did you know Sunday brunch is a pretty popular activity in New York? It was fucking crowded and I ended up eating at the bar (fancy that). The bartender (Jason) was fucking adorable (Tom gets the hots for a bartender - shocking!) and when he ducked under the bar and his pants, which were already slipping down his hips fell even further, well let's just say my dick doubled and so did his tip.
- Whoever it was I traded IM's with this afternoon while I was on my East Village walkabout, that was kind of cool. I'd love it if you used my MSN E-mail to let me know basic info. Who/where you are and such. Or just post a comment here. Speaking of mobility I'm going to open up my laptop to try and find out if there's a loose wire that's causing my screen display malfunction. If it is I can fix it. If the LCD is fragged I'll just get a new laptop once I go back to work.
- I found a book I ran across during a previous side trip to Barnes & Noble. I didn't buy it then and couldn't remember the title. But on my most recent visit I stumbled on the same book's sequel. A skinny homosexual helped me find book one. Fat White Vampire Blues. I'll let you know.
- We got mice. again. We get them periodically. I have the unfortunate job of buying, deploying and disposing of mouse glue traps.
- I'm really enjoying taking care of Colby. I've been finding a lot of comfort in having him curled up next to me, whether it's sleeping or just watching a movie on TV. He's taken to waking me up when he believes I've slept enough by standing on my chest and staring at me. Today we went to the dog run in Tompkins Square (read: lean Latinos with tatts). The on again/off again boyfriend punked out on taking Colby for the weekend. He was sick and hadn't slept. Just as well, I'm trying to get him on a schedule ( Colby, not the boyfriend).
That's the best I can do, folks. I'll try and post some better shit the rest of the week
Image via « groeg »
When good puppies go bad...
Mighty is right. Go Fug Yourself is stoopid funny.
Singer Robbie Williams accused of "drug-fueled homosexual act". Is there any other kind? But seriously, if this wanna-be a star in America Brit-pop poofta wants to play the "sexually confused" card at his age (what is he, George Michael?) I say we call him a bad fag and kick him to the curb. It's 2004, Robbie. If you suck dick you suck dick.
I just needed a day to think. Actually, to tell you the truth I spent one day in denial and recovering from a chemical and liquor fueled blackout. Recovering is probably the wrong word. I woke up, puzzled as to how I got home or in my bed. I remember speaking to The Ex, confused about whether it was the same day or the next. I think I actually walked the dog, but at best it felt like a hiccup in time. One second I was asking for another martini, the next I was home.
So, fired from a job I had grown to hate, and was intending to quit in a month. (My aforementioned big surprise.) And still I find myself resentful. I know almost none of it is about me. Frank, the German/Floridian has the Overlords' ear right now. They needed to provide him with a job and I had the job they needed. While I don't believe in self aggrandizement, which probably contributed to a lot of misconceptions about what was going on, I do believe in striving to be honest with myself. I know I did a good job. I was responsible, honest, available and a problem solver. I wasn't afraid to make a decision or address a difficult issue. I always admitted when I was wrong. I never based anything I did on anything other than what I thought was fair, best for the business or occasionally to be left alone. Worrying about protecting my job or showing how important I was didn't enter the picture. Perhaps it should have, but protecting a job that I never felt compensated enough for seemed, well.... stupid. Besides, I believe in doing a good job. I believe that if you do a good job that good things will come of it. I know, I'm an ass.
I got this long story about how they wanted someone who was more out on the floor mixing with the crowd but that's all bullshit. This was mostly about my inability to kiss ass and work the system. The Overlords really need their asses kissed. I have had more than one person say if I'm thinking it, I may as well have "fuck you" tattooed on my forehead. I used to be better at "playing the game", as I got older, as what I believed to be important in life changed I just couldn't (or wouldn't) pretend that stupid people , incompetent people, ridiculous people,... weren't. That can make you unpopular. It can apparently get you fired.
It's been years since I've been fired. That's not a good feeling. The oddest part of the experience was knowing in advance I was being fired. And then going to the main office, to be fired. "Hi, I'm here for you to fire me." Very odd. I guess preferable to having no idea. But I know how the Overlords think, I know how they operate. It's almost laughable what they believe they're accomplishing versus what's actually happening. How they've eliminated the last line of defense between order and utter chaos.
So it's done. Finished a month before I planned. But finished nonetheless. I can't wait to see the results of the only person who was actually doing things on a regular basis being pulled from the picture, but I'm not egotistical enough to think that a business that's been running for 15 years will somehow crumble in my absence. I'll be a blip on the history of the business before you know it. It will go on. I will go on. I hope I'll be missed by the people that matter to me.
So for now, I've decided to take a week to decompress. They've been paying me illegally off the books for the last three years so a sweet free ride on unemployment isn't an option. Fortunately, I was preparing to leave anyway so I'm not without my resources. But I'll have to find a new job sooner rather than later. I have some projects I've been meaning to tackle around the house. First up, the kitchen needs a major cleaning. Before I start that though, it's positively gorgeous outside. I think I'll put my nipples to the wind and head out..... there, somewhere. Want to meet me for brunch?
I was fired yesterday.
I'm heading to the new Home Depot.
More later .... I have time.
I spent the better part of this afternoon waiting for UPS. (Memo to UPS advertising department: Who the fuck green-lighted the "Brown" campaign? Repeating "brown" over and over is positively scatalogical. I can't believe over the course of however many meetings between corporate and advertising not one person raised a hand and said "Um, about this whole brown idea....".) When it's a delivery, I just make sure I'm home by 5 pm. This block is on a late afternoon delivery schedule which means that whatever you order will arrive sometime after 5, usually closer to 6:30. Now with all that tracking software they've added there's no more waiting for a delivery. Once you have the delivery date, if you happen to be privy to your neighborhood delivery schedule, you spend and hour usually waiting for your package. (he he "package" he he) Not so with pick-up, however. And I was waiting for UPS to pick up the defibrillators The Hellcat had sold. You read that right. It seems that one night shortly after he had moved in, The Hellcat was returning from somewhere East (village) of here, possibly the boyfriend's but just as likely not, when he came upon what appeared to be a wholesale dump of a medical office. There were chairs and lights and fixtures, those chrome tree thingys you hang IV bags off of. The thing that really caught his eye though was that there seemed to be several defibrillators just laying out in the trash, presumably waiting to be picked up to become so much landfill. Surely, he thought they couldn't be throwing away working defibrillators, but by the same token, they looked to be in pretty good shape so maybe.....
Which is how it came to pass that The Hellcat ended up returning to our apartment sometime well after 1 am lugging a discarded defibrillator. It was then I expressed my doubt that anyone would be careless enough to discard a working defibrillator onto a Manhattan street for anyone to find it and possibly be badly injured or killed by it's (mis)use. In retrospect I should have known better. In Manhattan we throw out desks, chairs, halogen lamps by the thousands. The microwave we threw out worked (badly). We throw out working computers with the hard drive still in them. Need a new monitor? You can wait if you like someone will throw one away eventually. Clothes that I don't donate I leave on top of the garbage to try and avoid a wholesale rummage. Hell, we even throw newborn babies into the trash on occasion. So would a working defibrillator be that much of a surprise? OK then, would three working defibrillators give you pause? Because when The Hellcat returned home and bravely (or foolishly, take your pick) plugged it in and fiddled with enough knobs to confirm that what we had here was a working defibrillator, he decided that it might have some resale value, and returned to the street where two more were waiting to be picked up. So for the last month or possibly longer it's been impossible to open The Hellcat's bedroom door all the way as it was being door-stopped by two defibrillators. And yes, we both had several thoughts/dares about trying them out (only at 20 joules or so) and speculations as to possible sex toy uses. Speculation, I assure you.

As the weeks went by The Hellcat talked to various medical equipment re-sellers and buyers and he had price quotes all over the map. It was clear that if he put a few days effort into it he could probably realize a quick thousand out of the deal if not more. But as we've seen these past few weeks, a few days effort, in succession, is beyond The Hellcat's abilities right now. A phone call on the subject per day was about all he could usually manage.
Which is how I ended up spending the afternoon waiting for UPS to pick up two of the three defibrillators. While he didn't manage to sell them outright, The Hellcat found a middleman who was willing to sell them on a more or less consignment basis. This was all finalized concurrent to packing for the trip, fooling around with the on again/off again boyfriend, trashing the apartment and sleeping through the original flight.
Be that as it may he made it to California, albeit a full 12 hours late. I'm down to one defibrillator, so if the whole building goes into cardiac arrest, someone's gonna die.
I apologize to anyone who took my Instant Messenger invite and didn't get a reponse. The IM's were forwarding to my phone and it's just too hard to log on and text answers that way. I still am not getting IM's to show up on my PC and I'm not sure why..... (to be investigated)
I ordered a new color Palm. The Zire 31. The next step up includes a camera but that's what I use a camera for. I think phone cameras and Palm cameras are stupid. Anyway they list for $149 but I found it on Overstock.com for $100ish and then used a $25 credit I was carrying on Paypal. Meaning the total cost to me was $86 and change. I still use my Palm M125 for the phone numbers and to-do list mostly. A color version will be nice. (to be anticipated)

I think I'm getting fired today. One of the Overlords called me in for a 4 pm meeting this afternoon. Is it at all surprising that the healthy, organized, hard-working, stable employee is getting the ax? Not with this bunch of lunatics. (to be continued....)
Sean Cody will pay me to carry the link.
The New York Times has an interesting article covering the first Manhattan Home Depot complete with concierge. I heart New York. A second location is due to open in December right on the corner of the street where I'm working now, but the first one will open this Friday. It's fascinating though, how they've seemingly thought of everything from stock delivery to customer checkout to best serve the urban home improvement crowd. I don't know how best to illustrate how excited I am about this, but I will say that my inner lesbian has a very wet pussy right now. Want to meet me Friday for lunch?
I was exploring the possibility of adding Google AdSense ads to my site. I thought it would be fun to try and maybe a way to generate some extra cash. It all seemed okey-dokey, until I got to their program policies page. I believe I lose on several fronts:
- Excessive fucking profanity.
- Illicit drugs and drug paraphernalia (thanks, Hellcat.)
- Pornography, adult, or mature content. Check, check and you betcha.
I wonder if Sean Cody will pay me to carry his banner?
I've managed to add internet access on the new work computer. Mischievously, I password protected it so Jabba The Drunk won't be able to get on. In my defense, he's a self-confessed porn junky, and my Verizon roaming access is for a set amount of hours after which I pay. And I'll be damned if I'm going to squander my substandard wages for that.
Speaking of Jabba, he's due back from a two week vacation tomorrow. I'm pleased to report the children behaved fairly well in his absence. I busied myself tricking out the new computer and sending a series of (mostly ignored) requests to my Overlords. I'm waiting to get approval to order up a DSL line. On a more important note, I managed to run the joint for two weeks predominantly on my own and I'm happy to say we always had liquor, change and ice. For a hootch-hole, that's pretty much a win. Update: I can report a late night liquor-fueled but not drunken confession wherein the temporary and disturbing (to me) German/Floridian manager that has been with us for the summer is not returning to Florida after all. Also that he doesn't like me. (Most people don't at first.) What this bodes for Jabba, me and the future is anybody's guess. Quite frankly I don't care, except in a detached, bemused sort of way. (Maybe that's why people don't like me.)
Speaking of The Hellcat, his 3 week vacation starts tomorrow. And let me just say that I have never seen a man more ill-prepared for a vacation in my entire life. He has virtually no money, he is without much needed prescription medication and as of 5 pm today he hadn't even begun packing. He has a small (legit) business deal that done right, would have funded the majority of the trip. Instead, it's being slapped together at the last minute with no guarantee that it will come together at all in his absence. Maddeningly, he's known about all of this for weeks. On yet another side note, it was understood from the begining that Colby would be going along on the trip. How unsurprised are we that the last minute attempt to secure his travel fell through as well and he's staying behind with yours truly playing the part of secretly delighted Auntie? Update: I returned home at 3:30 am to find The Hellcat simultaneously packing and sorting even more crap that he salvaged from a friends move. Literally moving things out and in to the apartment at the same time. The sink was absolutely full of dirty plates, glasses and dishes. There were clothes, household decor, packing material and medical equipment scattered all over the house. Unbelievably, he invited his on again/off again boyfriend over at that time. To help? Doubtful. I ended up doing the dishes, although the boyfriend offered to take over. Finally, I just fixed myself a bedtime cocktail and shut the door. It's now heading towards 1 pm. The flight has long since taken off. The Hellcat (and possibly the boyfriend) aren't even up yet. There are newspapers and half-packed boxes as well as luggage scattered throughout the house. In spite of being truly annoyed I feel profoundly sad that he's so severely damaged he can't manage to plan and execute a vacation.
The Ex is preparing to leave for a long weekend in North Carolina. It's the continuation of his, I Plan To Reach Retirement And Become A Burden To My Family And My Government Tour. He will accomplish this by seeing that he constantly pisses away every dollar he could potentially save, on trips and travel he neither needs nor can afford.
The Hellcat is in full preparation for an extended (21 day) tour of California, Vegas and Seattle. I'm excited for him as his last few trips out west have been related to illness and death, and this one is completely pleasure and family and reconnecting with same. That's always a good thing.
So I'll be without The Ex from today until Tuesday and then all alone every day in my spacious 3 bedroom Gramercy Park apartment most weekdays in September. Whatever is a girl to do? Note to self: Buy lube and camera batteries.
Excellent piece via The Stranger.com on why John Kerry and co. are experiencing a major disconnect with American voters. I'm firmly in the ABB (anybody but Bush) camp and I'll vote for virtually anybody who runs against him, but I'll be holding my nose as I flip that lever for Kerry.
Bush's acceptance speech -via glassdog
In other news:
My financial fortunes appear to have taken a turn for the better. It appears my country mouse existence may be coming to an end. If things stay on track and my time frame plays out as I've imagined, you can expect a surprise (well, not to me obviously) around the beginning of October. Stay tuned, kiddies.
As I do periodically I've made some changes to my little corner of the blogiverse. The first is a minor change courtesy of Blogger. If you scroll down to the bottom of any post you'll see a little mail type icon. Clicking on that will take you to an e-mail page, so if I say or do or post anything you think might amuse someone or give them needed information there will be no need for that time consuming control + "c", right-click "paste" business. I mean, who has time for that, right?
The second change is experimental. Because my spankin new cell phone came with AOL E-mail already enabled on the phone I decided to go for it and sign up for an AOL E-mail account. I'm not a big fan of AOHell (In the interest of full disclosure I do, however, own TimeWarner stock.) By default this includes being able to reach me at times via AIM. When I have it turned on. I could just make it a trifecta and sign up for Yahoo! and then tie the whole thing together using Trillian but that seems too geeky even for me. Besides, I'm not sure how much instant access I'm prepared to give y'all. As much as I have no objections to blurting out the details of every pimple on my shaved white ass, up to now, I've had most of the control as to how close you got. So for now, I make no promises. If you scroll down to the mailbox below my links section you'll find my AIM info. Please, I'm not trying to discourage you from using it. I'm eager to speak to some of you, as I've been trying (and mostly failing) of late to encourage more interaction with whoever is reading. Just understand in advance if I'm not home to respond or I need to keep a conversation brief. I may be heading out the door or not caffeinated enough to speak at length. We'll give it a try, though.
On another tangent entirely we went to what was dubbed a "peaceful candlelight vigil" in Union Square tonight. It started around 8 pm and when we arrived about 8:20 the entire Square was almost full and surrounded by police. The Hellcat and I had stopped off at a 99Cent store and bought boxes of candles to light and give away. Sure enough, as soon as we started giving them out it became apparent that we could always use more. So off went The Hellcat back to the store. He returned with boxes upon boxes of small tapered candles to give out to whoever needed one. We lit and highlighted ourselves in a semi-circle of various votives and tealights. We then proceeded to pass out candles to anyone who wanted one. We soon attracted photographers to document the scene. Extraordinarily, people not only used our votive setup to re-light their own candles, but they took the time to restore the flame to any of the votives that blew out from the breezes. My candle, of course was a martini glass with a candle instead of liquor inside. You know it's true! We billed ourselves as Alcoholics Against Bush. We chanted, we rapped, we laughed. The HRC rented a billboard sized truck emblazoned with the phrase "George W., You're Fired!". That drew a huge cheer. A FOX News van stopped at a traffic light in front of the Square. That drew a huge collective chant of "Fox News Sucks!" until the light changed and everybody laughed and cheered as it pulled away. We drew video coverage when they started a chant from a rap song I didn't know. Not to worry, I got into a call and response groove with a couple of guys on the other side and a sistah behind me. Apparently, rapidly aging white men who can manage a simple rap is worthy of videotaping. Go figure. And see that's what separates us faggots from the rest of you and always will. We don't just show up to a vigil. We work it. We got the vigil style. One part social protest one part "look at me!" And thus it has always been. It was just nice to finally feel, after practically being held hostage in our own city by this invasion of Repugnantans, that we did a little something to take some of the energy back. Now if you would all please return to Fat Doughy Whiteville or whatever backwards jerkwater 1st cousin marrying town you came from, we'll get back to minding everyone else's business and judging you and laughing. It shouldn't take long to forget you. Where did I put that martini shaker?
The Diagnosis and Treatment of Depression in HIV-Infected People
By Ross Slotten, M.D.
Depression is the most common psychiatric disorder in the United States. According to the National Institute of Mental Health, 10% of American adults, or nineteen million people over the age of eighteen, suffers from some sort of depression every year and a third of the adult population will experience a major depressive episode in their lifetimes. The incidence of depression in individuals living with HIV is twice as high. This is not surprising, since depression occurs at higher rates in all groups of people with chronic illnesses. The economic costs of depression in terms of lost time at work and medical care are considerable; but the greatest effects are on health. In patients with HIV disease, severity of depression correlates with rapidity of decline in CD4 counts, suggesting that a failure to treat depression may accelerate HIV disease progression and impact survival. Thus, depression can be as serious as certain co-infections, like hepatitis B and C.
Although there has been considerable progress in our understanding of the brain, the ultimate cause of depression is unknown. Even the role of certain neurotransmitters like serotonin is still unclear, despite intense marketing by the pharmaceutical industry. The hallmark of depression is an alteration in mood, but there are physical symptoms as well. Psychiatrists have identified ten symptoms of depression, which include the following:
- persistent sad, anxious or empty moods;
- feelings of hopelessness or pessimism;
- feelings of guilt, worthlessness or helplessness;
- loss of interest in pleasurable activities like sex or hobbies;
- decreased energy, fatigue or feeling "slowed down";
- difficulty concentrating, remembering or making decisions;
- sleep disturbances (insomnia, frequent awakenings or oversleeping);
- appetite and/or unintentional weight changes;
- thoughts of death or suicide or suicide attempts; and
- restlessness and irritability.
If five or more of these symptoms are present every day for at least two weeks, then a person is suffering from a major depressive episode. If the depressed moods and two or more of the above symptoms persist for at least two years, then the person is diagnosed with a dysthymic disorder (an antiquated term derived from the Greek, meaning diseased mind -- in this case, representing mild, chronic depression). If in addition to one or more major depressive episodes, the person experiences wild mood swings in the opposite direction -- that is, inflated self-esteem, grandiosity, pressured speech and so-called "flight of ideas," and abnormally high energy -- then he or she is said to be bipolar.
Diagnosis
Complicating the diagnosis of any mood disorder is substance abuse, which not only can mask underlying mental illness but can also mimic one mood disorder or another. Crystal methamphetamine, for example, elevates a person's moods to the height of mania, until the person crashes and appears profoundly depressed. Chronic use can lead to depletion of serotonin, which may result in permanent depression unresponsive to antidepressant medications. Crystal methamphetamine attracts depressed individuals because it creates a temporary sense of well-being and high energy, counterbalancing the low self-esteem and other debilitating somatic and cognitive symptoms of depression. After ingestion, this drug can also produce intense anxiety and palpitations or chest pain; patients frequently request antianxiety medications like Xanax or Valium to calm their nerves. Frequent requests for such medication should raise suspicions of substance abuse. In some studies, nearly three quarters of HIV-infected individuals who abuse drugs and alcohol suffers from some sort of psychiatric disorder, including depression.
Despite clear-cut criteria for diagnosing depression, depression is not always easy to diagnose or manage. Patients present with headaches, fatigue and weight loss, just as people do with other illnesses. If depression is suggested as a cause, they may insist that something else is wrong. In HIV-positive patients, the diagnosis of depression is especially tricky because they may indeed have serious underlying disease. But unless a person has end-stage AIDS or is on the downward slope of uncontrolled HIV infection, most HIV-positive people are relatively healthy -- the various nonspecific symptoms that they are suffering from may be due not to a deadly opportunistic infection but to depression. Yet ruling out other causes may be greeted with resistance or skepticism. It is ironic that, because of the stigma attached to mental illness in our country, people would rather be told that they have some dreaded disease than depression.
The public still does not equate psychiatric disorders with organic disease -- diseases of the mind seem less legitimate than pneumonia or lymphoma. A blood test, CT scan, MRI or an X ray will not diagnose depression; it remains a clinical diagnosis, after other diseases have been ruled out. And treatment is no easier. The prevailing belief is that depression can be solved by a change in attitude, finding a new job, moving to a new city, or ending a relationship -- all of which may happen without improvement in symptoms before the true problem is addressed. In the meantime, the patient is lonely, unhappy and living in strange surroundings without adequate emotional support. Moreover, the notion of psychotherapy or antidepressants repels most people, even though depression is a treatable condition, unlike the dreaded disease the patient thinks he or she has.
As mentioned, other diseases should be ruled out before diagnosing depression. First and foremost is advancing HIV infection. Patients with declining CD4 counts and rising viral loads may exhibit a few of the characteristics of depression, such as fatigue and weight loss. If the patient has never been treated for his or her HIV infection, or the patient with resistant disease has remaining treatment options, then highly active antiretroviral therapy (HAART) should improve symptoms in a few weeks. AIDS-dementia, now rare, may also present as a depression-like illness. In more subtle cases, neuropsychiatric testing -- a battery of written and oral testing by a specially trained psychologist -- must be conducted in order to distinguish between organic brain diseases like HIV encephalopathy and a mood disorder. Unlike depression, dementia progresses over time, with profound impairment of mental processes, radical personality changes, and eventual alterations in levels of consciousness before death.
Two other medical conditions should be considered before treating depression: hypogonadism and hypo- or hyperthyroidism. Hypogonadism, or abnormally low testosterone levels, may cause fatigue, weight loss and depressed moods. For reasons that are unclear, impairment of testosterone production is common in HIV-infected men. Testosterone deficiency is defined as a total serum testosterone
Finally, a number of anti-HIV medications have so-called neuropsychiatric side effects. The most infamous in the category of antiretroviral agents is efavirenz (Sustiva in the U.S. and Stocrin in some other countries), which can cause an array of symptoms, from vivid dreams to mood-altering states mimicking depression. AZT (Retrovir) and abacavir (Ziagen) can produce extreme fatigue, loss of energy, and depression. Cause and effect are usually obvious, occurring within days or weeks of initiation of therapy. When the patient finds these side effects intolerable, stopping the medication resolves the problem; persistence suggests another reason for alterations in mood. Many other agents used to treat a variety of non-HIV related problems can also depress mood or induce somatic complaints, but the list is too long to enumerate in this article.
The management of depression in HIV infection is usually multidisciplinary, involving psychologists, social workers and psychiatrists. The primary health care provider rarely has the time or expertise to provide the full scope of services to the depressed person. When substance abuse is a problem, access to a good treatment program with sensitivity to issues unique to HIV like sexuality is essential. In addition to restoring emotional health, major goals of psychotherapy are the prevention of the transmission of HIV to uninfected individuals or reinfection with a resistant strain of HIV, and adherence to the HIV-treatment regimen.
Most of the DHHS recommendations are common sense. Implementation of these recommendations, however, can be a challenge. The clinician must overcome a number of barriers to ensure proper therapy -- social, psychological and medical. Some of these barriers have nothing to do with the patient but everything to do with our health care system, which is fragmentary and driven by third-party payers. Yet until the creation of a comprehensive health care system in this country -- whether in the form of a single-payer, government-managed system, or one resembling the mix of government and private payers cobbled together by the Clinton administration -- certain barriers, such as access to affordable health care for the working poor, will be impossible to overcome.
First, the patient must be convinced that he or she is depressed, which, as already noted, is not always easy. Second, the patient must agree to see a psychotherapist, at least for an evaluation. For those who lack or have insufficient mental health benefits, access to less expensive or free mental health care varies from community to community. In communities offering such services, quality is not always consistent. Psychotherapy may span weeks or years, which is a significant time commitment; out-of-pocket expenses can be considerable, even for those having the most extensive insurance coverage. Gay patients often prefer to see a gay therapist, which HMOs and other managed health care plans may not be able to guarantee, though insurers have become increasingly sensitive to sexual orientation in recent years. In some parts of the developing world, psychotherapists do not exist; patients who emigrate from those countries may not be amenable to psychotherapy because they do not accept the Freudian or post-Freudian model of the mind. Thus, there may be cultural barriers that prevent patients from obtaining psychotherapy. Third, the primary care physician or psychiatrist may recommend prescription medication that patients are reluctant to take. Patients often resent the addition of yet another medication to an already burdensome regimen, or they may fear antidepressants, which they equate with mind-altering substances like LSD. They may also worry about side effects, especially the impact on sexual function.
Treatment
The pharmacological treatment of people with HIV and depression has been studied extensively, though not every drug available has been examined. The oldest class of antidepressants, the tricyclics (amitryptilline, imipramine, desipramine and nortryptilline), were the first drugs subjected to a scientific evaluation. Approximately three-quarters of patients given imipramine, for example, responded favorably as compared to 30% on placebo. However, almost a third of the patients stopped imipramine because of side effects, which include constipation, dry mouth, drowsiness, headaches, cognitive problems and sexual dysfunction. This is unfortunate, because tricyclics are inexpensive. Today, their role is limited mainly to the treatment of pain from peripheral neuropathy, which improves with a dose lower than that for depression. More expensive medications, like fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa) and a derivative of citalopram, Lexipro, which belong to the SSRI class (selective serotonin uptake inhibitors), have produced response rates as high as 90% in some studies. Side effects are relatively few, though sexual dysfunction, which is the most common complaint, occurs at rates higher than the pharmaceutical companies like to admit. Rarely are erections a problem; most aggravating is time to ejaculation. In this setting, Viagra, Levitra and Cialis are of no use, since these agents help only those men who have difficulty obtaining or maintaining an erection and do nothing to speed up ejaculation. Venlafaxine (Effexor), nefazodone (Serzone), buproprion (Wellbutrin) and mirtazapine (Remeron) -- the non SSRI antidepressants -- seem to cause less sexual dysfunction. In fact, bupropion is sometimes added to an SSRI-containing regimen to improve sexual function. Few studies with these agents have been conducted in HIV infected patients -- which does not mean they are not effective in this population. Moreover, there may be a significant interaction between these non-SSRI agents and antiretroviral regimens containing Norvir (ritonavir). These drugs should therefore be used with caution in patients on Norvir boosted PIs or Kaletra.
Psychostimulants, like methylphenidate (Ritalin), can also help patients who are suffering from depressed mood, fatigue and cognitive impairment. Their onset of action is more rapid than that of the tricyclics, SSRIs, and other antidepressants, which may take four to six weeks before maximal benefit is observed. Ritalin works in a matter of hours; but its abuse potential is high and tolerance to its effects typical. Annoying side effects include overstimulation and insomnia; and for those who are concerned about maintaining weight or lipodystrophy, amphetamines suppress appetite. This class of drugs works best in patients with end-stage disease or in those whom the clinician suspects adult attention deficit disorder, a syndrome whose symptoms are difficult to distinguish from chronic anxiety disorder as well as depression. Finally, St. John's wort should be mentioned. Although shown to be effective for mild depression, St. John's wort negatively interacts with indinavir (Crixivan), making regimens containing indinavir less effective. Its interactions with other protease inhibitors are unknown. St. John's wort should not be used in patients taking HIV medications until further studies support its safety and efficacy.
In conclusion, depression is a common, treatable problem in people with HIV infection. It may be due to a condition long preceding HIV infection or to substance abuse; or it may arise in the course of infection, either as a result of HIV medications, illnesses, or the overwhelming emotional response to HIV itself. If not treated or recognized, it can profoundly affect quality of life and life expectancy. Clinicians, patients, their families and significant others should suspect depression when there is no other explanation for depressed mood, fatigue, or other vague somatic complaints that impair social functioning. Psychotherapy and the appropriate use of antidepressant medications can restore such individuals to normal emotional health, which, by curtailing self-destructive behavior and improving adherence to antiretroviral regimens, will help ensure a long, productive life.
About me
- I'm Tom
- From New York, New York, United States
- I've recently come to the conclusion that I'm no crazier than most people. It was a relief. I've spent the better part of 40 years twisting my life into a giant ball of anxiety and character flaws. I intend to spend the next forty unraveling it. And then dropping dead.
- My profile
Last posts
Recent Comments
Archives
- 04/01/2003 - 04/30/2003
- 05/01/2003 - 05/31/2003
- 06/01/2003 - 06/30/2003
- 07/01/2003 - 07/31/2003
- 08/01/2003 - 08/31/2003
- 09/01/2003 - 09/30/2003
- 10/01/2003 - 10/31/2003
- 11/01/2003 - 11/30/2003
- 12/01/2003 - 12/31/2003
- 01/01/2004 - 01/31/2004
- 02/01/2004 - 02/29/2004
- 03/01/2004 - 03/31/2004
- 04/01/2004 - 04/30/2004
- 05/01/2004 - 05/31/2004
- 06/01/2004 - 06/30/2004
- 07/01/2004 - 07/31/2004
- 08/01/2004 - 08/31/2004
- 09/01/2004 - 09/30/2004
- 10/01/2004 - 10/31/2004
- 11/01/2004 - 11/30/2004
- 12/01/2004 - 12/31/2004
- 01/01/2005 - 01/31/2005
- 02/01/2005 - 02/28/2005
- 03/01/2005 - 03/31/2005
- 04/01/2005 - 04/30/2005
- 05/01/2005 - 05/31/2005
- 06/01/2005 - 06/30/2005
- 07/01/2005 - 07/31/2005
- 08/01/2005 - 08/31/2005
- 09/01/2005 - 09/30/2005
- 10/01/2005 - 10/31/2005
- 11/01/2005 - 11/30/2005
- 12/01/2005 - 12/31/2005
- 01/01/2006 - 01/31/2006
- 02/01/2006 - 02/28/2006
- 03/01/2006 - 03/31/2006
- 04/01/2006 - 04/30/2006
- 05/01/2006 - 05/31/2006
- 06/01/2006 - 06/30/2006
- 07/01/2006 - 07/31/2006
- 08/01/2006 - 08/31/2006
- 09/01/2006 - 09/30/2006
- 10/01/2006 - 10/31/2006